Swallowing difficulties (dysphagia)
Swallowing difficulties can make it hard for you to eat and drink. They can be caused by a wide range of conditions, some of which can be serious.
On this page
- Causes of swallowing difficulties
- Symptoms of swallowing difficulties
- Diagnosing swallowing difficulties
- Dietary suggestions for swallowing difficulties
- Food and drink thickness levels
- Safe eating and drinking
- Safe eating and drinking with facial weakness or numbness
- Safe eating and drinking with thinking or memory difficulties (cognitive impairment)
- Treating swallowing difficulties
Causes of swallowing difficulties
Problems with swallowing can range from mild to severe. Any stage of swallowing can be affected. This can be from getting food and fluid into your mouth and throat, and down through your food pipe (oesophagus) into your stomach.
They are usually caused by another health condition and can happen at any age.
Common causes of swallowing difficulties include:
- some medicines, such as antipsychotics
- heartburn and acid reflux
- cancer, such as mouth or throat cancers
- nervous system or brain disorders, such as multiple sclerosis, Parkinson's disease, dementia, a stroke
- muscle disorders
- blockages or structural issues with your mouth, throat or food pipe.
Symptoms of swallowing difficulties
Symptoms of swallowing difficulties may include:
- coughing or choking when eating or drinking
- bringing food back up, sometimes through your nose
- a feeling that food is stuck in your throat or chest
- a gurgly, wet-sounding voice when eating or drinking.
You may also drool and have problems chewing your food.
Over time, swallowing difficulties can cause weight loss, dehydration and repeated chest infections.
Diagnosing swallowing difficulties
Let your healthcare provider know quickly if you have swallowing difficulties. They will ask you about your symptoms and check if any other health conditions may be the cause.
Your healthcare provider may refer you to a specialist for tests. These may include a:
- gastroscopy — a tiny camera is passed down through your mouth to look at your throat and stomach
- swallowing study — your mouth and throat are x-rayed as you swallow small amounts of food and fluid.
Videofluoroscopic swallowing study
If you are struggling to maintain a healthy weight, you may need to see a dietitian. A dietitian can help you make sure the food you are eating is well-balanced, nutritious and has the right consistency.
Dietary suggestions for swallowing difficulties
If you have problems swallowing, your speech-language therapist may recommend that you change the consistency of your food and fluids (drinks). This is to help you eat and drink better and more safely.
If you have dentures and they fit well, always wear them when eating. If your dentures are loose, this may be due to unintended weight loss — you may need new dentures or other help to prevent further weight loss or to regain lost weight.
The International Dysphagia Diet Standardisation Initiative (IDDSI) is an international standard for food and fluids for people with swallowing difficulties.
The IDDSI uses a framework with different levels to describe how thick a drink is or how soft a food needs to be.
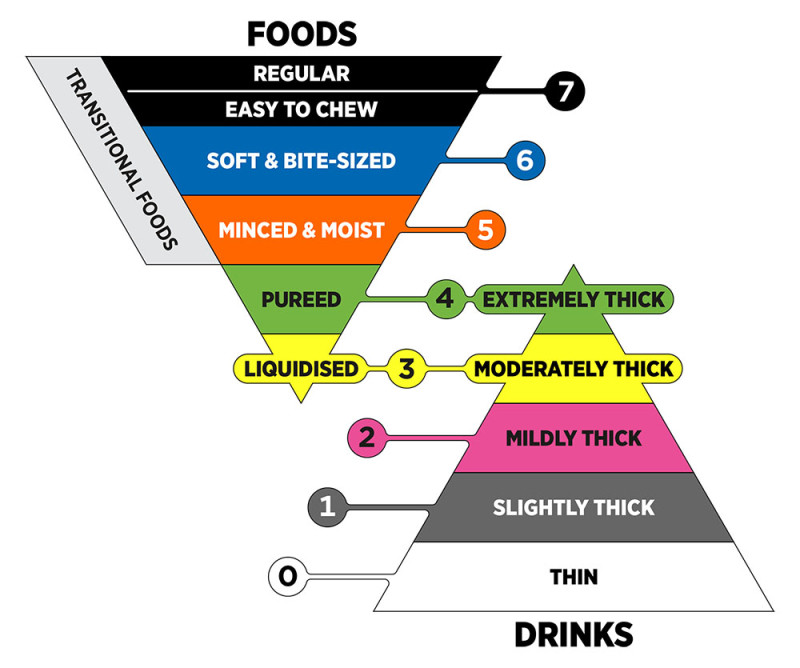
The International Dysphagia Diet Standardisation (IDDS) framework. © The International Dysphagia Diet Standardisation Initiative 2019. CC BY-SA 4.0
If you have swallowing difficulties, your speech-language therapist will assess you. They will work out what levels you need for food and fluids. When you know which levels to use, refer to the corresponding leaflets below.
Only use the leaflets after getting advice from your speech-language therapist. Do not change to a different level without first checking with a healthcare provider.
Go to the International Dysphagia Diet Standardisation Initiative website for the most up-to-date information and resources.
International Dysphagia Diet Standardisation Initiativeexternal link
The food leaflets have information about testing. The testing is to make sure your food has the right consistency.
If someone else prepares your food, they will make sure the consistency is right. If you prepare your food, you can use the tests. When you get used to preparing your food, you will probably not need to do the tests every time.
The fluids leaflets also have information about testing. If you prepare your fluids, you will probably not need to do the testing yourself. You will usually follow instructions given to you by your speech-language therapist. They will tell you how much thickener to add to the fluids.
Some of the fluid tests measure how much liquid is left in a syringe after 10 seconds of flow. If you want to find out about flow testing, the International Dysphagia Diet Standardisation Initiative (IDSSI) has a series of videos to watch.
IDDSI testing methods for drinks — YouTubeexternal link
Thickening fluids
If you have problems swallowing, your speech-language therapist may recommend that you thicken fluids to make them safer to swallow.
Watch this video to see how thickener works:
Thickening fluids — Vimeoexternal link
To thicken your fluids:
- Read the instructions on your thickening product to see how much you need for your consistency level.
- Measure your fluid as per the product information.
- Add the required amount of thickener.
- Stir briskly with a fork for 30 to 40 seconds.
- Leave to thicken if the product instructions tell you to.
Call your pharmacy and ask them to order the thickening product for you. Make sure you specify the product name you would like ordered.
You can also purchase them online. Products include:
- Altrix Superior Thickener
- Flavour Creations Instant Thick
- Nutricia Nutilis Powder
- Precise Thick-N-Instant.
Safe eating and drinking
If you have difficulty with your swallowing, you can be at risk of food or drink entering your airways. There are some things you can do to help make eating and drinking safer.
- If you get tired as the day goes on, eat your main meal earlier in the day.
- If you have dentures and they fit well, always wear them when eating.
- Concentrate fully on eating and avoid talking.
- You might find it easier to eat several small meals rather than 3 larger meals.
- Track your weight. Check it at least once a month to make sure you are eating enough and getting enough calories.
- If you are concerned about weight loss, talk to your healthcare provider or your dietitian.
- Try to avoid dry food, such as cornflakes, coconut and pastry, as it can catch in your throat.
- Changing the consistency of some food may make it easier to swallow. You may be able to cut it into smaller pieces, mash it, mince it or purée it.
- Adding extra sauces and gravies to savoury food or custard and whipped cream to sweet food may make it easier to swallow.
- You might have to swallow twice for each mouthful.
- If your voice is gurgly when you eat, give a small cough to make sure your airway is clear.
- Foods that have 2 consistencies (such as peaches in juice, soup with vegetable pieces or cereal floating in milk) might be harder to swallow. Eat the solid food by itself, then have a spoonful of the liquid. If you can, stir the food into one consistency. For soups, blend them first.
- Smooth brown bread may be easier to swallow than white bread.
- Room temperature water is generally harder to swallow. You may find it easier if all your drinks are hot, ice-cold or fizzy.
- If you have been advised to have thickened fluids, avoid jelly and ice cream, as they melt into a thin liquid before you swallow them.
- To avoid tipping your head backwards, try drinking thin liquid from the top half of your cup only.
- If your voice is gurgly when you eat or drink, give a small cough to make sure your airway is clear.
Try the following suggestions to see if they help. If you still have difficulties, discuss them with your healthcare provider.
- Sit upright in a chair. It is best to sit at a table.
- Avoid talking and other distractions, such as television, while eating or drinking.
- Take small mouthfuls of food and liquids (bites or sips). It may help to use a teaspoon.
- Have a strong swallow to help move the food or liquid.
- After swallowing, do extra swallows until your mouth and throat are clear. Wait before putting more food or liquid into your mouth.
- Try alternating a sip of liquid with mouthfuls of food. If this makes swallowing more difficult, try avoiding liquids with meals.
- Check that your mouth is clear at the end of meals. Use your tongue or a clean finger to clear food from your cheeks. You may need to clean your teeth and mouth.
- Stay sitting upright for half an hour after you have had food or liquids.
Ask your healthcare provider if you can do anything else to make eating and drinking easier.
Find a therapist — New Zealand Speech-language Therapists' Associationexternal link
Dietitian services — Healthpointexternal link
Safe eating and drinking with facial weakness or numbness
Some conditions, such as brain injury and stroke, can cause muscle weakness, shortness of breath and tiredness (fatigue). This means it can take longer to eat a meal.
The following tips may help to make eating easier and safer.
- Keep food to a soft, moist consistency such as mince, mashed potato, steamed fish, soft vegetables and soft fruits such as avocados and bananas.
- Avoid dry and very fibrous or dense foods that need a lot of chewing, such as steak, crackers, biscuits, toast and toffees.
- Sucking on an ice cube before you eat may improve sensation and make it easier to eat.
- Take a sip of water or other drink between each mouthful of food. This can help to clear any food that is left behind in parts of your mouth that you cannot feel.
- Clear your cheek with your tongue or a clean finger during and after eating to make sure food does not remain in your cheek.
- Having a drink after a meal will also help to clear any remaining food out of your mouth.
- Remember that if you cannot feel one side of your mouth properly, you are more at risk of biting your cheek. Take extra care.
Safe eating and drinking with thinking or memory difficulties (cognitive impairment)
Cognitive impairment means a person has trouble:
- remembering
- learning new things
- concentrating
- making decisions.
It can range from mild to serious, and often happens after a stroke or brain injury, or with dementia.
If you care for someone who has these difficulties, the following strategies might make mealtimes easier.
Offer meals at regular times of the day. The person may find it easier with 5 or 6 small meals rather than 3 larger ones. Let them eat when they are hungry.
Try to prepare familiar foods in familiar ways, especially their favourite foods.
Set up the table so they are looking at someone else eating, as this may remind them to eat and swallow.
Make sure:
- they are seated upright
- they are not sleepy or tired
- any distractions are removed (turn off the radio or TV, limit visitors, close the door)
- they can see the food and drink
- they have their special cup or cutlery
- you present one food item at a time — main, then dessert, then a drink
- you encourage them to feed themselves whenever possible. You can help by putting your hand over theirs
- you remind them to follow any guidelines given by the speech-language therapist.
If the person you are helping holds food in their mouth for too long, try serving foods that may help prompt them to swallow. These may include sweet, sour, spicy, hot or cold foods. Be careful with hot food.
If they are eating too quickly, remind them to slow down. Encourage them to put their spoon or fork down on the plate between mouthfuls. Offering them smaller cutlery, such as a teaspoon, can help to reduce the size of each mouthful.
If you need to feed the person, first follow the advice above.
And if the person cannot see the food or liquid:
- describe what they are eating or drinking
- ask 'are you ready?' and tell them when you are giving them another mouthful.
When you are feeding them:
- sit in front of them (rather than to the side)
- make sure they have swallowed each mouthful before offering another. You can watch to see if their Adam's apple has risen and fallen, or check that the food has gone from their mouth
- allow time for them to swallow more than once
- use a teaspoon if they can only have small mouthfuls
- stop feeding them if they become tired, sleepy or have any difficulties, such as coughing or being unable to clear their mouth
- make sure their mouth is clear and clean after meals — you may need to clean their teeth and mouth.
There are many different strategies to make eating and drinking safer. Talk to your speech-language therapist if you have any questions or concerns.
You may also want to access private specialist help.
Find a therapist — New Zealand Speech-language Therapists' Associationexternal link
Treating swallowing difficulties
How your swallowing difficulties are treated depends on the cause and how severe it is. Treatments may include:
- medicines to treat acid reflux
- swallowing therapy with a speech-language therapist
- making changes to what you eat and drink, such as softer foods and using thickener in drinks
- using special spoons, plates and cups
- surgery to widen your food pipe (oesophagus).







